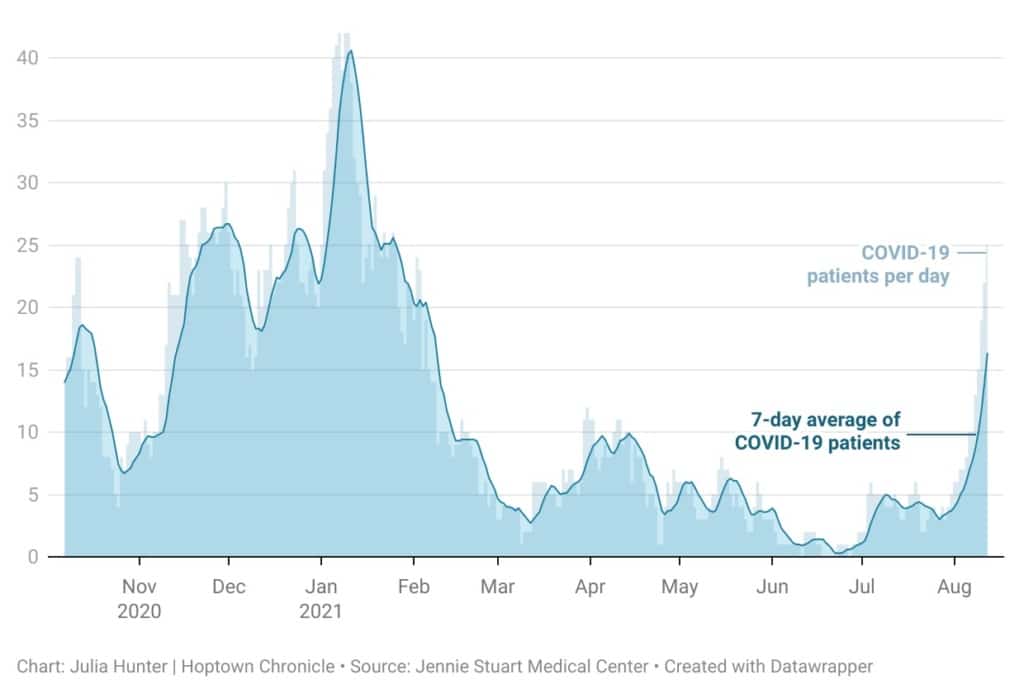
In the last two weeks, COVID-19 hospitalizations at Jennie Stuart Medical Center have skyrocketed — increasing more than 500%.
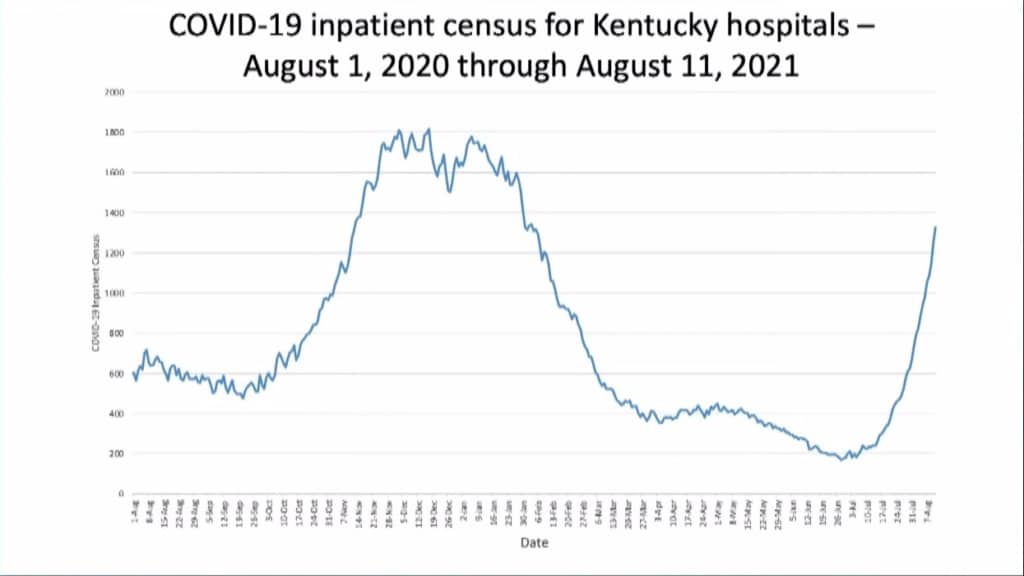
It’s a trend being seen across the commonwealth, as the highly contagious delta variant drives a surge in cases that Kentucky Public Health Commissioner Dr. Steven Stack has called “the fastest and steepest rise in cases of the entire pandemic.”
Less than two months after Jennie Stuart marked the first day in a year without any patients hospitalized with the virus, COVID-19 admissions locally and statewide have returned to levels last seen in February. But then, they were going down. Now, they’re increasing at a pace that is concerning public officials and health care leaders.
On Thursday, 1,371 COVID patients were hospitalized statewide. At Hopkinsville’s only medical hospital, there’s been a “constant influx” of coronavirus patients recently, said Beth McCraw, vice president of nursing and clinical services at Jennie Stuart. Two weeks ago, there were just four COVID patients hospitalized at Jennie Stuart. As of Thursday morning, there were 25. It’s the sharpest local increase since the pandemic began.
As health care workers grapple with the pandemic’s most recent wave, a few things are clear: patients hospitalized with COVID are getting sick quicker, are younger than before and are mostly unvaccinated.
Not a ‘slow go’
McCraw told Hoptown Chronicle that during the initial waves of the pandemic, “you could pretty much mark the calendar” about 10 to 14 days after a community spike in positive cases, and there would be a spike in hospital admissions. Then, about 10 days later, there would be a spike in patient deaths.
Now, patients who require hospitalization end up being admitted in about half the time — around five to seven days after testing positive, McCraw said.
“It is not taking as long for a person to get sick enough to be admitted,” she said.
“We’re ramping up a lot quicker. This surge that we’re seeing is not a ‘slow go.’ It’s really a very ‘fast go.’”
It’s a dynamic that puts even more strain on hospital staff, which has been the most valuable — and limited — resource in the fight against COVID-19 since the beginning of the pandemic.
During a press conference on Thursday, Gov. Andy Beshear pointed to what’s happening in states just south of Kentucky as examples that “ought to be ringing alarm bells throughout this commonwealth.” As hospitals across Mississippi fill up with COVID-19 patients, health care leaders warn that the medical system statewide could be on the verge of failing without drastic intervention. Earlier this week, Arkansas reported just eight unoccupied ICU beds in the entire state.
Some areas of Kentucky are already seeing hospitals fill up. In Morehead, St. Claire Health Care is in the process of opening a “surge ICU” because its intensive care unit is full, the hospital’s chief medical officer William Melahn said Thursday, joining the governor’s press conference remotely.
Many health care facilities are also seeing an increase in overall patients, including many who haven’t tested positive for the virus, but need urgent medical attention.
“With this new wave, we have the benefit of knowledge gained, but we now have the difficulty of our non-COVID patients being more ill than they were before, as many of them prolonged seeking treatment for their illnesses due to the pandemic and our rising COVID numbers,” Miriam Haas, the nurse manager at Norton Brownsboro Hospital in Louisville, said during Beshear’s press briefing on Tuesday.
Federal data show a similar trend at Jennie Stuart. During the seven-day span from July 29 to Aug. 4, 640 patients visited the hospital’s emergency department — more than any other time during the entire pandemic, according to a hospital-level capacity report from the U.S. Department of Health and Human Services. The total includes patients who visit the emergency room for any reason, including those who receive treatment for COVID-19 but weren’t admitted — a metric not reflected in the hospital’s daily COVID-19 hospitalizations.
From July 30 to Aug. 5, there also were more inpatients beds occupied at Jennie Stuart than any time in the last six months.
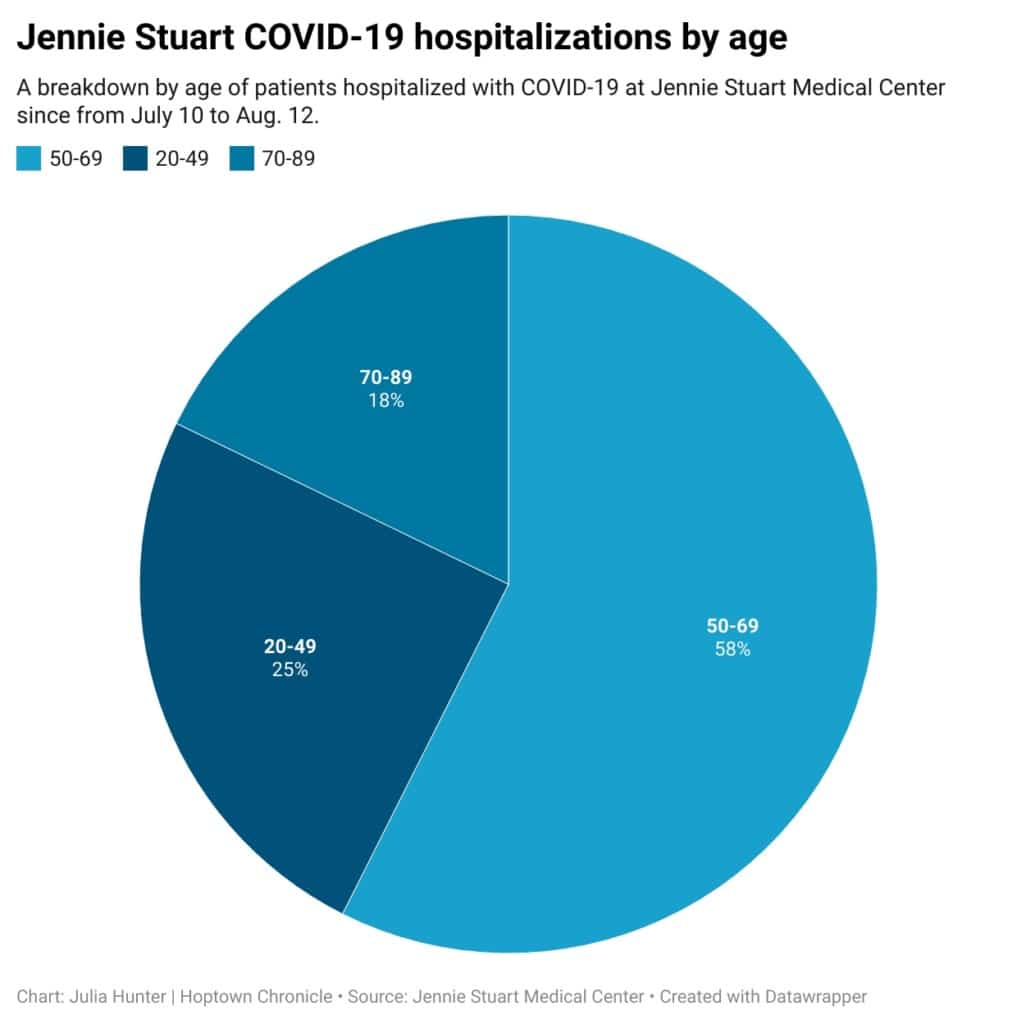
Increase in younger COVID hospitalizations
One-fourth of all COVID patients hospitalized at Jennie Stuart since July 10 have been between 20 and 49 years old, according to hospital spokesman Chris Jung.
It’s twice the share of individuals in the age range who were hospitalized with the virus during the first six months of the pandemic, according to data previously provided by Jennie Stuart.
Some health care professionals across the country have coined a new phrase — “younger, sicker, quicker” — to describe how the delta variant has differed from the original strain of the disease.
“These past few weeks, as we have been seeing more patients with the delta variant, we have had to deal with a new problem: younger patients who become unstable more unpredictably,” Haas said during the press conference Tuesday. “These patients tend not to have any other illnesses that contribute to their sickness. They don’t really have anything in common with each other except that they have the delta variant and many of them are not vaccinated.”
McCraw, who said patients hospitalized recently at Jennie Stuart don’t necessarily appear to be sicker, did agree the illness is progressing faster and the age of patients is much broader than it was early on. During the first phases of the pandemic, the majority of patients hospitalized with the virus were in the “older middle-aged group,” she said. In recent weeks, they’ve ranged anywhere from their 30s to their 90s.
A common thread: lack of vaccination
McCraw, like many other health care workers across the country, said there is one characteristic that the vast majority of COVID patients hospitalized at Jennie Stuart have shared: They’re not vaccinated.
Since July 10, just two of the hospital’s COVID-19 admissions have been vaccinated, according to data provided by Jung.
“I know there’s still a lot of hesitation for the vaccine. But … something that we have seen here — and it’s followed suit with what the nation is seeing as well — out of all these patients that we have in the hospital with COVID, today we have just one who has been vaccinated,” McCraw said Wednesday afternoon, when there were 23 COVID patients hospitalized at Jennie Stuart.
“I really would like to put the plea out that, if people can, we really do encourage people to get the vaccine. It’s safety for them. It’s safety for their loved ones. And it’s important for the community.”
As of Thursday, just 24.27% of Christian County residents had received at least one dose of the vaccine, compared to the statewide average of 54%. The county’s vaccination rate is the fourth worst in the state.
Hospitals shift (again) to adapt to new surge in cases
The recent surge in cases has prompted some area hospitals to postpone or cancel elective surgeries and other non-urgent procedures, a move Beshear noted on Thursday that hospital’s “won’t do unless it’s really, really serious.”
Last week, Vanderbilt University Medical Center in Nashville announced its adult hospital is once again rescheduling surgeries that can be delayed, as a result of the influx.
Others, like UK HealthCare and Jennie Stuart, have decided to limit the number of people inside their facilities to protect patients, staff and visitors.
On Thursday, Jennie Stuart announced updated visitation guidelines. The primary change was the limitation of visiting hours, said Jung. With the exception of the maternity and emergency departments, visitation will only be allowed from 9 a.m. to noon. It’s a shift from previous guidelines updated on May 26 allowing visitation from 8 a.m. to 7 p.m. The local hospital is not currently postponing any elective procedures, Jung said.
On Thursday, Stack reminded Kentuckians that they should still seek medical care at the hospital if they have an emergency.
“Please, do not stay home and avoid getting emergency care if you feel you have an emergency,” he said during the governor’s press briefing. “On the flip side, if you have an optional or elective or non-urgent in-patient procedure scheduled in the next few weeks, if you were my family member, I would encourage you to reschedule it. The next month is not a good time to be in a hospital. The staffing ratios are going to get stretched and it is not a good time to be in a hospital if you do not have to be.”
Julia Hunter is the engagement editor for Hoptown Chronicle. Reach her at julia@hoptownchronicle.org.