State inspections of Kentucky nursing homes since the coronavirus pandemic began found almost no deficiencies in infection control, though nursing-home residents have accounted for more than 60 percent of the state’s 524 deaths from COVID-19, John Cheves of the Lexington Herald-Leader reports.
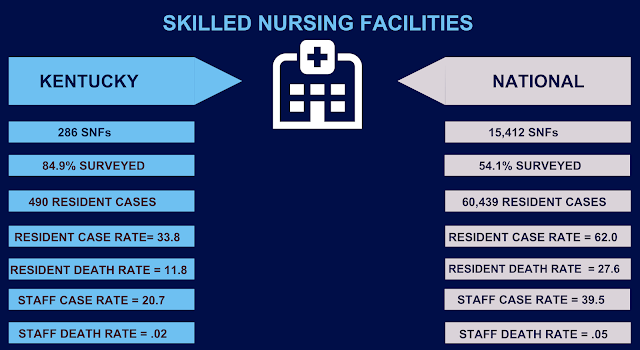
“Covid-19 has reached at least 57 percent of Kentucky’s 285 nursing homes,” Cheves reports. But from March 10 through June 16, “The Kentucky Health and Family Services Cabinet identified deficiencies in only 3 percent of the 202 inspection reports it had released.”
“How could it be that everyone is doing such an excellent job that we can’t find deficiencies, and yet all of these residents are getting covid and dying?” asked Toby Edelman, senior policy attorney for the Center for Medicare Advocacy in Washington, a lobby for care of the elderly and disabled.
One big reason appears to be that inspections became cursory when the pandemic hit, under orders from the U.S. Centers for Medicare and Medicaid Services. It ordered states to inspect all nursing homes at least once by July 31 or risk losing part of their coronavirus-relief funds, Cheves notes.
And rather than the usual multi-day tours by inspectors, he writes, “CMS has limited covid inspections to one or two people filling in boxes on a “streamlined review checklist” of questions, such as: Do employees wear masks properly? Do they wash their hands and have easy access to disinfectant? Has the facility ended communal dining and other group activities?”
And, to reduce the time spent in nursing homes, which are closed to visitors to prevent infection, inspectors are encouraged to follow up with phone interviews with managers” rather than have “face-to-face conversations throughout the facility,” Cheves reports.
Infection control is the main problem in nursing homes, and Kentucky’s numbers are near the national average, patient advocate Edelman told Cheves. He reports, “Her group published a study last week finding that only 2.83 percent of infection-control surveys of nursing homes nationwide have identified deficiencies during the pandemic.”
Before the pandemic hit, Cheves reports, 41% percent of Kentucky’s nursing homes were cited for infection-control deficiencies.
The object example of Cheves’s story is Ridgewood Terrace Nursing Home in Madisonville, where 24 of the 100 residents have died of COVID-19 in the last three months.
“Like nearly one-fourth of Kentucky nursing homes, Ridgewood Terrace entered the pandemic rated ‘much below average’ in its quality of care” by CMS, Cheves reports. “State inspectors cited it over the last three years for poor infection control, resident abuse, failure to report abuse and inadequate staffing. It paid nearly $75,000 in civil fines in 2018. But on April 7, following an infection-control survey, the Office of the Inspector General at the health cabinet published a short, tersely worded report finding ‘no deficient practice identified’ at Ridgewood Terrace.”
The cabinet replied, “Facilities with a large number of deaths or a large number of positive cases cannot be cited on the grounds of an outbreak.” Cheves writes that the agency “refused to comply with an Open Records Act request by the Herald-Leader to provide copies of all deficiencies issued since March 1.”
Cabinet spokeswoman Susan Dunlap provided Kentucky Health News a copy of her overall reply to Cheves, which said, “Information on enforcement cases is not available through Open Records until the process is closed. For the eight facilities identified as having immediate-jeopardy deficiencies, the findings are pending CMS review and processing. Once this has been completed, they will be posted.”
More generally, Dunlap said the state “has been aggressive in its protection of residents and staff of these facilities. Visitation was ceased earlier than was the case in other states.” Also, “We have formed strike teams to provide immense ongoing resources to several facilities. (The Department for) Behavioral Health has provided resources to employees, in this time that has tested resilience.” … Purposeful action has been taken, and will continue to be taken, to help prevent the amplification of covid-19 in Kentucky’s long-term care facilities.”
Dunlap said “residents, family members, caregivers or others may file a complaint by phone or by email” with the Office of the Inspector General. “Even if the OIG is aware of who is bringing a complaint forward, the information is not shared with the facility.”
In other COVID-19 news:
- Gov. Andy Beshear reported 117 new coronavirus cases and two more covid-19 deaths Sunday, raising the totals to 13,750 and 526. The fatalities were a 73-year-old man from Butler County and a 61-year-old man from Fayette County. Beshear had not reported numbers on recent Sundays, when numbers are low partly because of limited reporting by labs, but resumed after federal officials asked for reports seven day a week. The new-case number was significantly higher than the two previous Sundays, when 85 and 70 cases were reported, but less than the 214 reported June 1, during a period when the state saw a surge of cases.
- President Trump’s aides said he was joking in Tulsa Saturday night when he told them to “slow the testing down, please” because it increases the number of reported cases. The federal government has little if any control over testing, a function supervised by the states.
- Kentucky has allowed restaurants to resume using tablecloths “as long as they are laundered between uses,” the Courier Journal reports. The revised requirements still urge restaurants to use disposable versions of products “to the greatest extent practicable.”
- U.S. Senate candidates in Kentucky are taking different approaches to seeking votes as the June 23 end of the primary election nears, the Lexington Herald-Leader reports.
- National Geographic answers the question, “How do I keep my kids safe as things reopen?”