The General Assembly is advancing a bill to remove out-of-pocket charges for follow-up diagnostic breast examinations and supplemental breast examinations when they’re medically necessary.
A scientific study has found that one in five women don’t get recommended follow-up breast exams because of cost.
- SUBSCRIBE: Sign up for our newsletters
The House Health Services Committee approved House Bill 115 on Feb. 1, and the measure was posted for passage in the full House on Monday, Feb. 5.
“This bill really is about early detection of breast cancer,” said Rep. Kim Moser of Taylor Mill, the bill’s primary sponsor and the committee chair. “It’ll ensure that individuals at high risk for breast cancer have access to diagnostic mammograms or follow up imaging. This is obviously needed to rule out breast cancer or the need for further testing.”
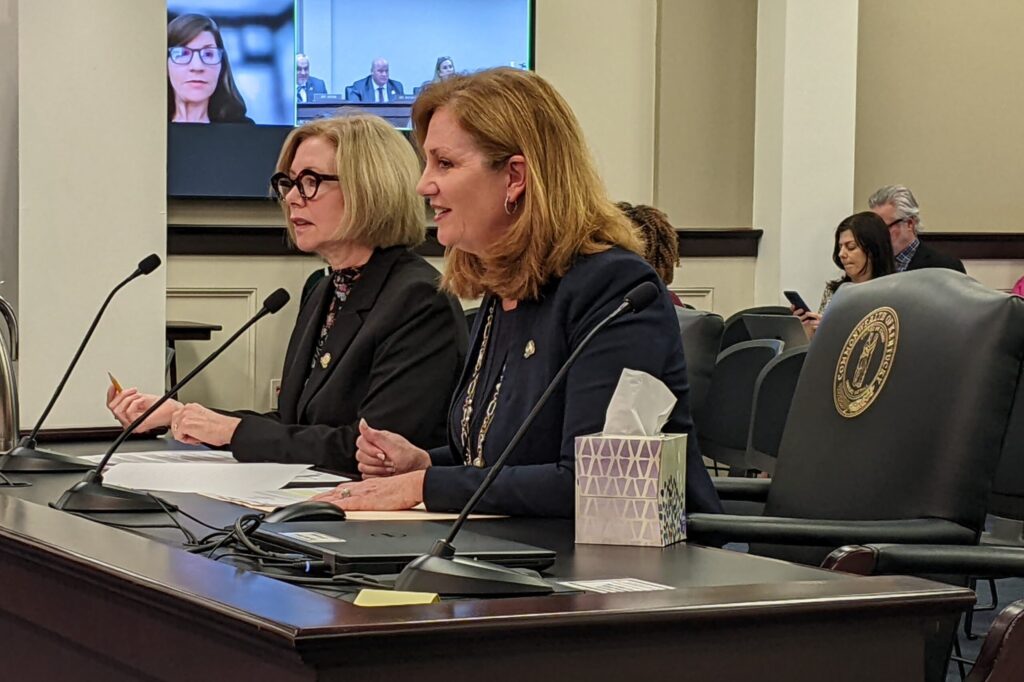
Rep. Lisa Willner, a Democrat from Louisville, presented the bill with Moser. Willner filed a similar bill last year that did not get any traction.
“The good news is that overall, our overall cancer numbers are declining,” Willner said. “But breast cancer is one of the areas that’s actually on the rise in Kentucky, really emphasizing the importance of this bill.”
Indeed, Kentucky’s breast-cancer rate showed a steady rise between 2005 and 2019, when it reached a high of 132 women with breast cancer per 100,000, according to the National Cancer Institute.
In 2020, the rate declined to 127 cases per 100,000 women, but that was a “temporary, anomalous year” because of the pandemic, according to NIC. The pandemic caused reduced cancer screenings and diagnosis, which resulted in a decline in the 2020 incidence rates for most cancer sites, the agency said.
The American Cancer Society estimates that one in every eight women will be diagnosed with breast cancer in her lifetime.
In 2023, more than 4,030 Kentuckians will be diagnosed with breast cancer and more than 790 will die of the disease, according to a letter from philanthropist Susan G. Komen supporting Willner’s 2023 bill.
Dana Carter, regional manager for state policy and advocacy for Komen’s breast-cancer foundation, explained to the committee members why the follow-up testing is needed and how it would remove financial barriers to medically necessary diagnostic and supplemental breast examinations.
“Mammography is only the initial step in the early detection process and it is not able to diagnose cancer alone,” she said. “Early detection of breast cancer is not possible without medically necessary follow up imaging or additional supplemental imaging which is required to rule out breast cancer or confirm the need for a biopsy.”
She said an estimated 12% of women screened with “modern digital mammography” will require follow-up diagnostic imaging.
Further, she noted that a Komen-commissioned study recently found that out-of-pocket costs for patients varied widely and are often high, adding to the stress and confusion for patients who need such tests.
“For example, the average patient cost for a mammogram is around $250, and for a breast MRI over $1000,” she said.
Carter also pointed to a study published in the scientific journal Radiology that found “one in five patients would not go in for the recommended follow up because they had to pay a deductible.”
“Unfortunately, we received many calls and emails from individuals who are unable to pay the out-of-pocket costs for the recommended follow up breast imaging,” she said.
“Without assistance, many simply will delay or forego these medically necessary tests. This can mean that patients will not seek care until the cancer is potentially spread, making it much more costly or in deadlier to treat.”
Carter added, “Breast cancer can be up to five times more expensive when it is spread beyond the breast to other parts of the body.”
The state Department of Insurance estimates that the bill would increase the cost of health insurance a as much as 57 cents per member per month, or not at all. “This represents an increase of approximately 0.0% to 0.1% or approximately $0 to $2.5 million for all fully insured policies in Kentucky, excluding Medicaid and state employees, due to the increased costs for health plans,” the department says.
The agency “acknowledges that there is a potential for long-term savings due to increased affordability and accessibility to cancer diagnostic testing which could lead to earlier detection of cancer.”
This story is republished with permission from Kentucky Health News. Read the original.
Melissa Patrick is a reporter for Kentucky Health News, an independent news service of the Institute for Rural Journalism and Community Issues, based in the School of Journalism and Media at the University of Kentucky, with support from the Foundation for a Healthy Kentucky. She has received several competitive fellowships, including the 2016-17 Nursing and Health Care Workforce Media Fellow of the Center for Health, Media & Policy, which allowed her to focus on and write about nursing workforce issues in Kentucky; and the year-long Association of Health Care Journalists 2017-18 Regional Health Journalism Program fellowship. She is a former registered nurse and holds degrees in journalism and community leadership and development from UK.






